Some countries are struggling to meet the 95-95-95 targets by 2030, including the Republics of the Philippines and Ghana. Without immediate change, these countries will continue to lag behind and fail to achieve international goals. Both countries teach us several lessons:
- Financial support from international and bilateral donors is not the sole ingredient to success.
- Partnerships and data-driven management are critical to running accountable programs.
- Governments and communities must implement policy changes with fidelity.
The Philippines: A once silent epidemic now out of control
HIV/AIDS came comparatively late to the Philippines, with the first cases only publicly identified in the mid-1980s. Over the years, several challenges have led to a rise in new infections. Testing and treatment have not been widely available in many parts of the country, and those most at risk for contracting HIV – young people, pregnant women, migrants, and injection drug users – have not been adequately reached:
- Adolescents between 15 and 18 years old needed parental consent to take an HIV test until 2019, testing of pregnant women was not routine, and violence against drug users drove many into hiding, likely contributing to the spread of infection.
- A lack of economic opportunity has led generations of Filipino men to migrate abroad for work and some return home with undiagnosed HIV.
- The national health insurance program did not include coverage for HIV prevention and treatment until 2019, a barrier to access to antiretroviral treatment (ART).
As a result, the number of new HIV infections in the Philippines has increased more than sixfold since 2010 (Figure 12). Estimates suggest the current HIV-positive population of 189,000 could more than double by 2030, even as the pandemic remains concentrated in groups at highest risk. Only 62% of Filipinos living with HIV know their status, and only 43% of those are on treatment. In a preventable tragedy, inconsistent linkages between testing and ART are producing an unusually high rate of AIDS-related deaths in young people.
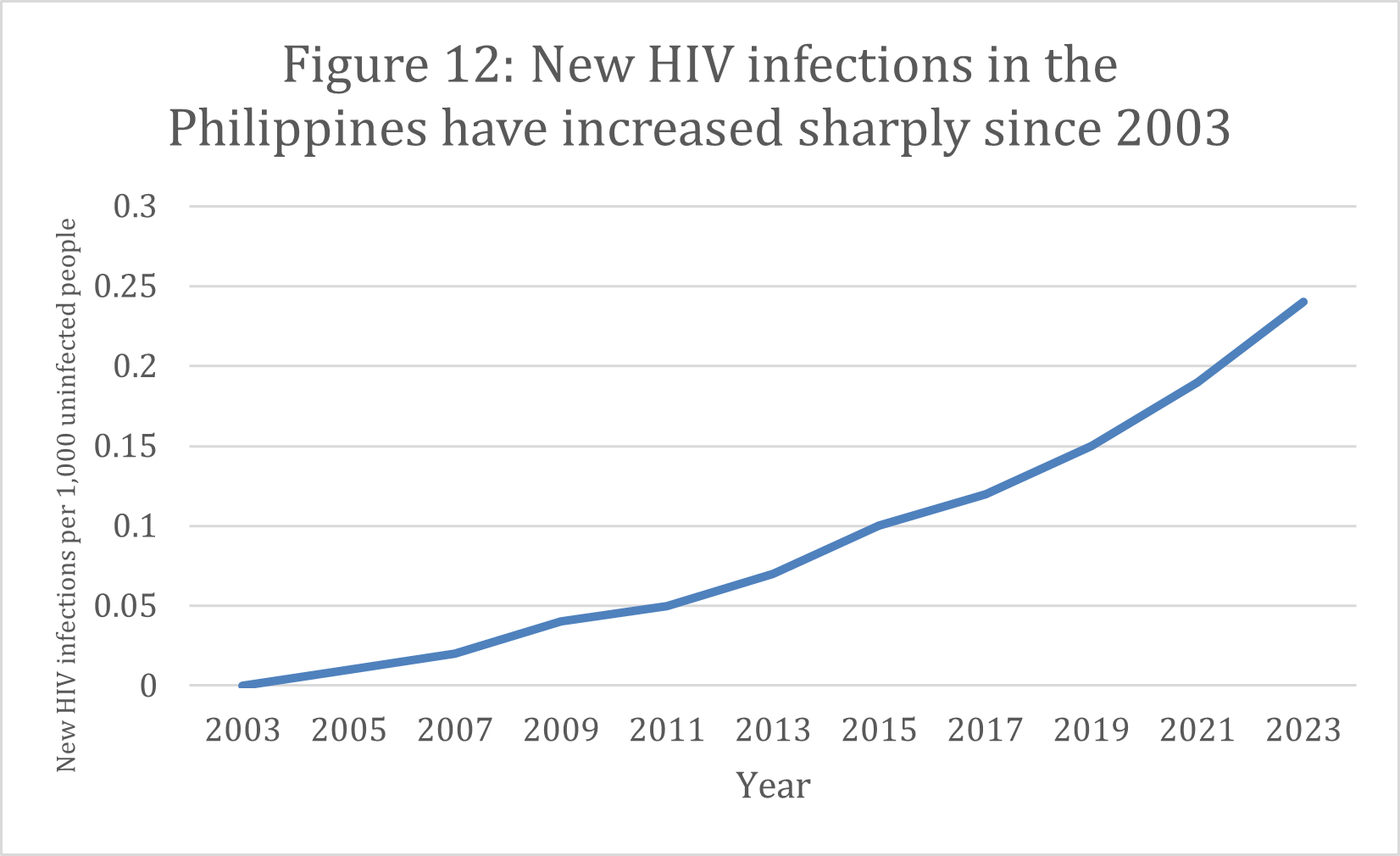
Source: UNAIDS
Seeing the rapid increase of new infections in 2016, the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) sent a team to the Philippines to review the situation. The team not only came back with clear data that confirmed a growing HIV pandemic but also found that the government needed to deepen its engagement with communities most at risk.
Despite these dire statistics, the government and local communities in the Philippines have a chance to save thousands of lives. To continue to make progress, the government of the Philippines and its partners must work in deep coordination with PEPFAR and community-based actors to ensure the most vulnerable are safe. Implementing lessons learned from similar outbreaks – such as providing access to more convenient testing options, reducing delays in returning testing results, and immediately enrolling diagnosed clients on treatment – will make HIV programming in the Philippines more efficient and contribute to a decrease in new infections over time.
|
Philippines |
||
| At least 95% of all people living with HIV should know their status (as of 2023) | At least 95% of all people with diagnosed HIV should receive ART and continue it (as of 2023) | At least 95% of all people on ART should have undetectable levels of the virus in their blood, known as viral load suppression (as of 2023) |
| 62% | 43% | -* |
*Not available at the time of publication.
Ghana: Missed opportunities
Ghana’s HIV epidemic resembles its sub-Saharan Africa counterparts. Most new infections are concentrated in the general population, with wide variation between regions across the country. The overall percentage of HIV-positive people remains relatively low at 1.5%, and ART has been available throughout the country for more than a decade through the country’s National AIDS Program, with financing from the Global Fund to Fight AIDS, Tuberculosis, and Malaria and technical and financial assistance from PEPFAR.
By all definitions, Ghana should have already reached the 95-95-95 targets. However, only 65% of people living with HIV know their status, and only 45% of HIV-positive people are on treatment. The annual number of new HIV infections in Ghana has declined by just 19% since 2010 – a stark contrast from the 39% decrease in Tanzania during the same time period (Figure 13).
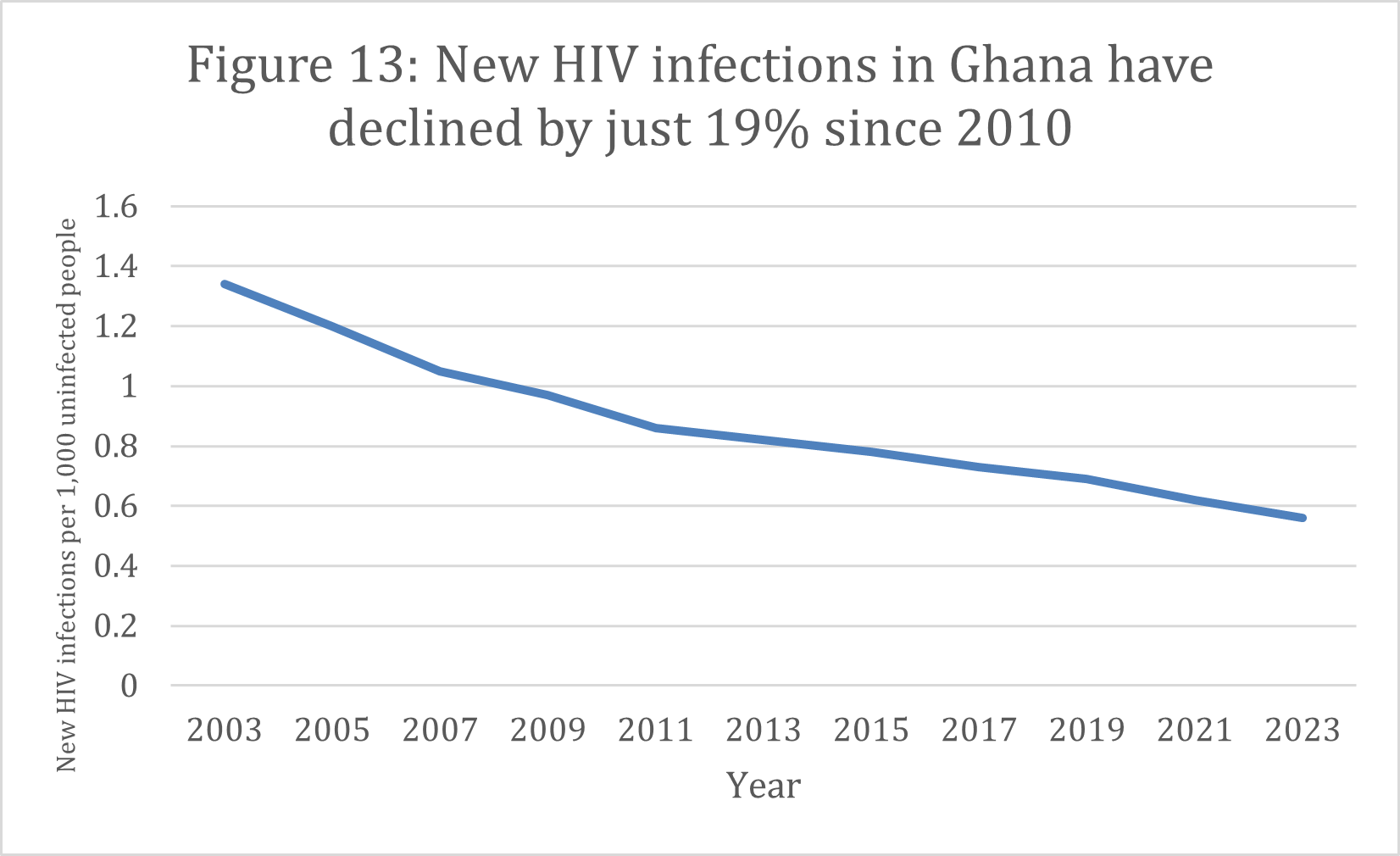
Source: UNAIDS
Several factors account for Ghana’s performance, all of which illustrate the importance of reforming policies and financing models while addressing barriers to care to end HIV as a public health threat. In Ghana, those living with HIV and members of the LGBTQ community are stigmatized and under threat, which discourages testing and treatment. Ghana has experienced challenges in decentralizing public-sector health services because of uncoordinated policies and limited input from district-level managers in the decision-making process. This has led to inconsistencies in the quality and availability of care across the country. And after almost 25 years, the Ghanaian government still has not met its commitment under the Abuja Declaration – a pan-African agreement to devote 15% of national budgets to health care. With limited funding invested in health, it will be difficult for Ghana to sustain the progress it has made against HIV.
These challenges can be addressed with the right political commitment and effective, data-driven management. The Ghanaian government should increase its budget for health, including funds dedicated for HIV. It should also pursue strategic partnerships with the private sector while better investing its resources by using real-time data to match needs. Health professionals at the district level should have more opportunities to influence policymaking and decide how to allocate human and financial resources in their areas, with a focus on eliminating barriers to care. Additionally, implementing evidence-based and permissive policies that protect human rights will be essential to ensure equitable access to health care and support for vulnerable populations.
Compassionate, quality care for HIV-positive people and their families requires continuous supportive supervision of providers and education campaigns led by national leaders to begin to reduce stigma. The adoption or expanded implementation of innovations, including peer counselors, heightened community engagement, intensive case-finding among key populations, convenient testing options, and multimonth prescriptions, would help more Ghanaians start and stay on ART.
|
Ghana |
||
| At least 95% of all people living with HIV should know their status (as of 2023) | At least 95% of all people with diagnosed HIV should receive ART and continue it (as of 2023) | At least 95% of all people on ART should have undetectable levels of the virus in their blood, known as viral load suppression (as of 2023) |
| 65% | 45% | 40% |

































