Several countries are on the right path to meet the 95-95-95 targets by 2030 due to support from the U.S. President’s Emergency Plan for AIDS Relief (PEPFAR) – including the United Republic of Tanzania and Vietnam – and can teach us important lessons:
- Reformed legal frameworks and policy reforms can create long-lasting changes in HIV epidemics driven by key populations.
- Programs must continuously focus on vulnerable populations and communities at the highest risk for contracting and spreading HIV.
- Course corrections are necessary when delays in policy reforms affect progress.
- Host-country health insurance schemes can provide clear fiscal sustainability.
Tanzania: Understanding data and people’s needs leads to progress
Early in the pandemic, the PEPFAR program in Tanzania used high-level country data that failed to show which regions had the greatest burden, leading to overinvestment in highly populated coastal regions and underinvestment in the highest-need areas.
The first Tanzanian countrywide HIV survey in 2016 collected data disaggregated by age, sex, and geography and showed that the percentage of people infected with HIV varied greatly by region. For example, HIV prevalence was about 11.4% in Njombe, compared with less than 1% in Lindi (a coastal region) (Figure 6).
Figure 6: HIV prevalence among people 15+ in Tanzania varies greatly by region (2016-2017)
Source: Tanzania HIV Impact Survey (2016-2017)
The country’s 2016-2017 impact survey funded by PEPFAR offered troubling evidence that Tanzania was at risk for a significant rise in new infections partially because of gaps in PEPFAR-funded programs. Only 52% of HIV-positive people in Tanzania were aware of their HIV status.
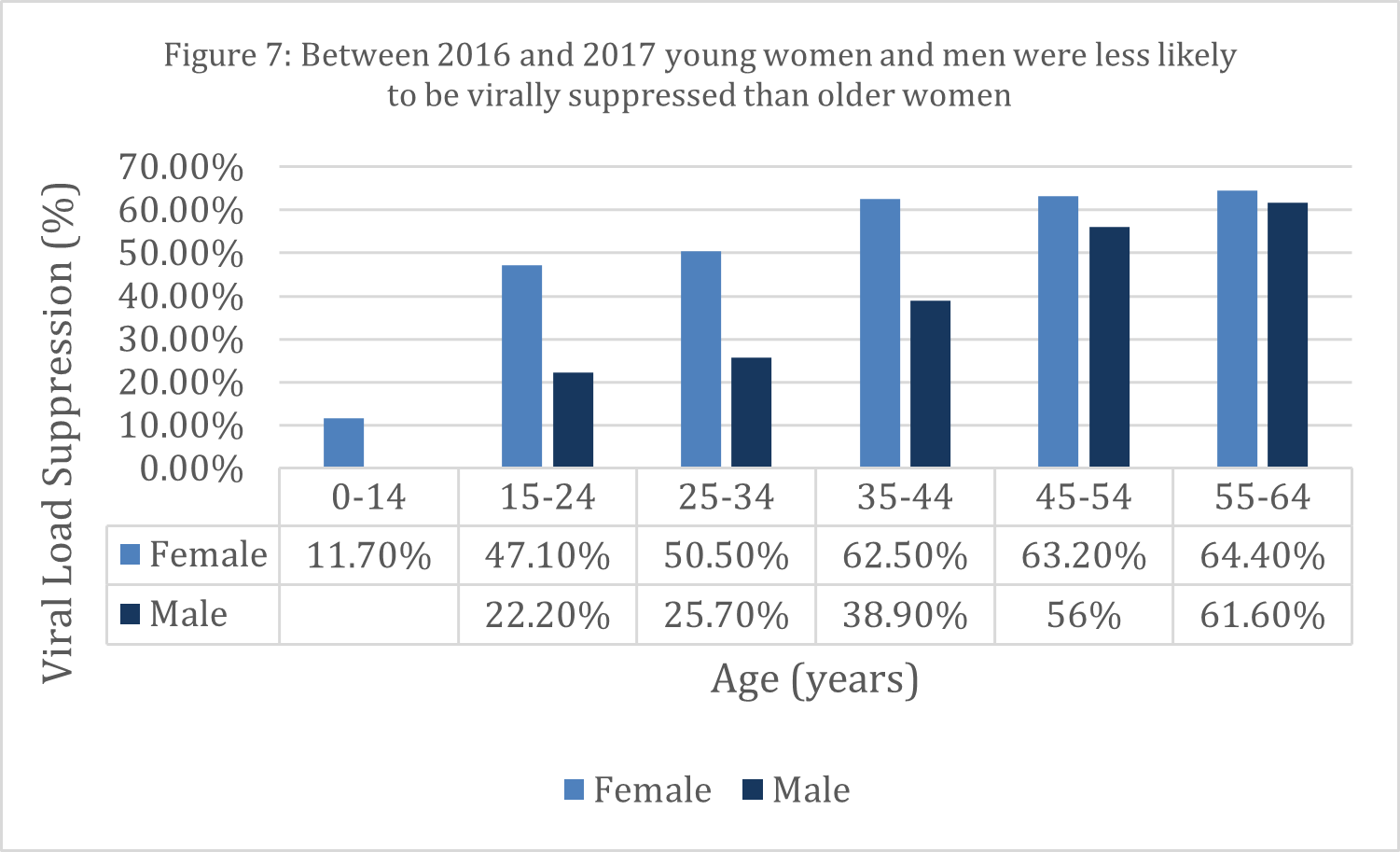
Disaggregated data were even more telling. Women were more likely to be tested for HIV and be on lifesaving treatment than men. Additionally, HIV-positive young women on antiretroviral treatment (ART) were less likely to be virally suppressed – or have undetectable amounts of the virus in their blood – than older women diagnosed and treated during pregnancy (Figure 7). As a result, Tanzanians diagnosed with HIV were at risk of developing HIV that was resistant to medication.
Source: ICAP
These surveys – now conducted routinely – have allowed stakeholders to see the urgent need for shifts in resources and investment. Recognizing the gaps between testing and treatment, PEPFAR made the difficult decision to change its investment strategy in Tanzania. The program directed resources toward populations and geographies that needed greater attention – specifically men in Western Tanzania and young women – by moving funds between partners and agencies in different regions. In just six years, the number of Tanzanians who knew their HIV status, started treatment, and achieved viral load suppression increased significantly, leading to a fall in new HIV infections (Figure 8).
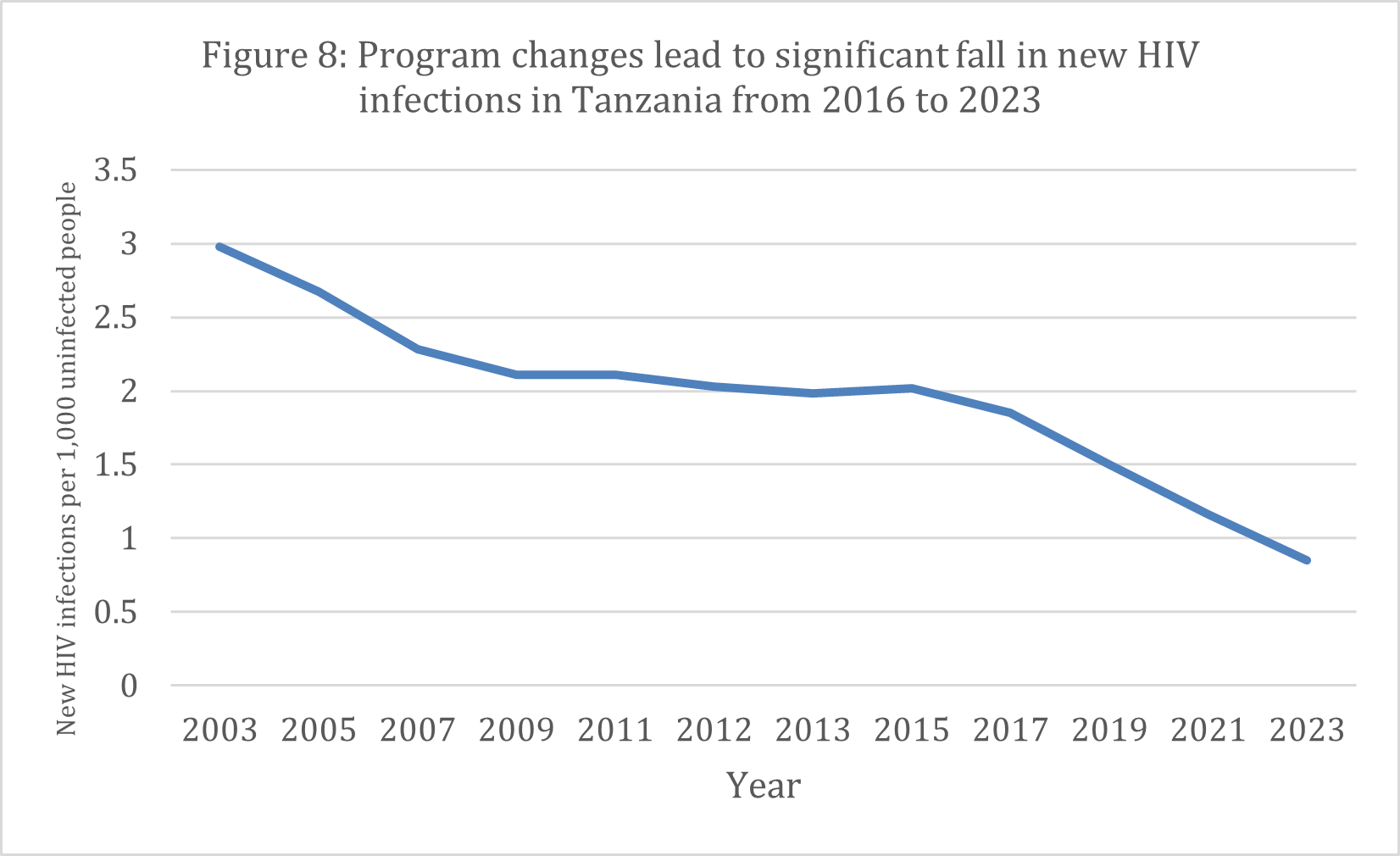
Source: UNAIDS
However, disaggregating the latest survey data by gender makes clear that women under 35 and men under 65 are still falling behind in Tanzania. The country’s overwhelmingly young population (median age of 19) provides a clear opportunity for improvement to ensure everyone not only survives HIV but thrives.
To achieve the 2030 goals in Tanzania, the national government must continue to modify its policies to ensure all its citizens in need of prevention and treatment services have access, including key populations and their communities. At the same time, PEPFAR must prioritize high-quality, data-driven, and data-validated programming that ensures mutual accountability.
PEPFAR, the Tanzanian government, communities, and private partners must focus on each community and age group that still requires direct attention. They can then invest in peer educators and community health workers who can reach and empower those in need of prevention, testing, and treatment to ensure that they remain on ART and achieve viral load suppression. Increasing the use of drugs that require fewer follow-up visits will help young, working age Tanzanians stay on treatment – potentially addressing the gap in ART coverage between the younger and older generations. Given that young men and women have the highest burden of disease, controlling HIV in Tanzania also requires the expansion of prevention activities like preexposure prophylaxis (PrEP) – medication used to prevent the transmission of HIV – voluntary male medical circumcision, and PEPFAR’s Determined, Resilient, Empowered, AIDS-free, Mentored, and Safe (DREAMS) program.
|
United Republic of Tanzania |
||
| At least 95% of all people living with HIV should know their status (as of 2023) | At least 95% of all people with diagnosed HIV should receive ART and continue it (as of 2023) | At least 95% of all people on ART should have undetectable levels of the virus in their blood, known as viral load suppression, (as of 2023) |
| 87% | 82% | 79% |
Vietnam: Critical national policy changes allow investments to reach key populations
Vietnam is an outlier of success in the fight to end AIDS as a public health threat by 2030, as advancement has stalled in many other middle-income countries, which have high rates of new HIV infections, low awareness of status, low treatment coverage, and low viral load suppression. Joint investment between PEPFAR and the Vietnamese government and substantial policy changes that reduce stigma and discrimination have been essential to the country’s progress.
Source: UNAIDS
*Key populations include those most at risk for contracting HIV (i.e., sex workers, men who have sex with men, people who inject drugs, transgender individuals, and people in prisons or incarcerated).
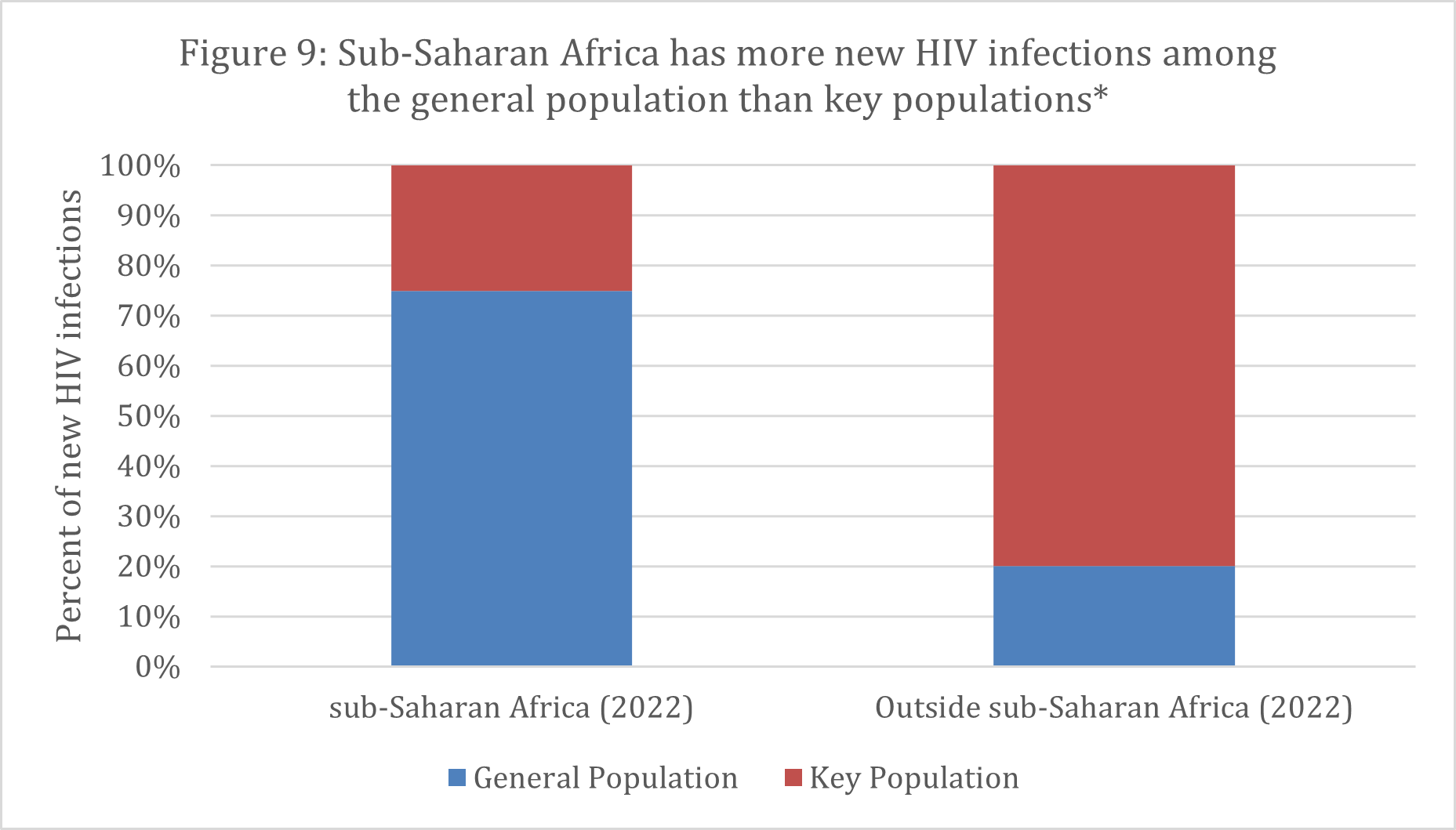
Sub-Saharan Africa has more new HIV infections among the general population whereas countries outside of the region have more new infections among key populations (Figure 9). In Vietnam, people who inject drugs and sex workers are at the highest risk for contracting HIV. Although they are in the greatest need of prevention and treatment services, many were often arrested, detained, and housed in specific centers 20 years ago. These arrests and confinements have decreased, partly thanks to diplomacy from the U.S. Embassy in Vietnam. Beginning in 2007, PEPFAR convinced the Vietnamese government to allow funding for prevention and treatment sites, including for drug-substitution therapy, and helped increase the number of peer educators and outreach workers. Slowly, a level of trust developed, and individuals at risk of contracting HIV enrolled in prevention services. Testing also expanded to reach vulnerable populations.
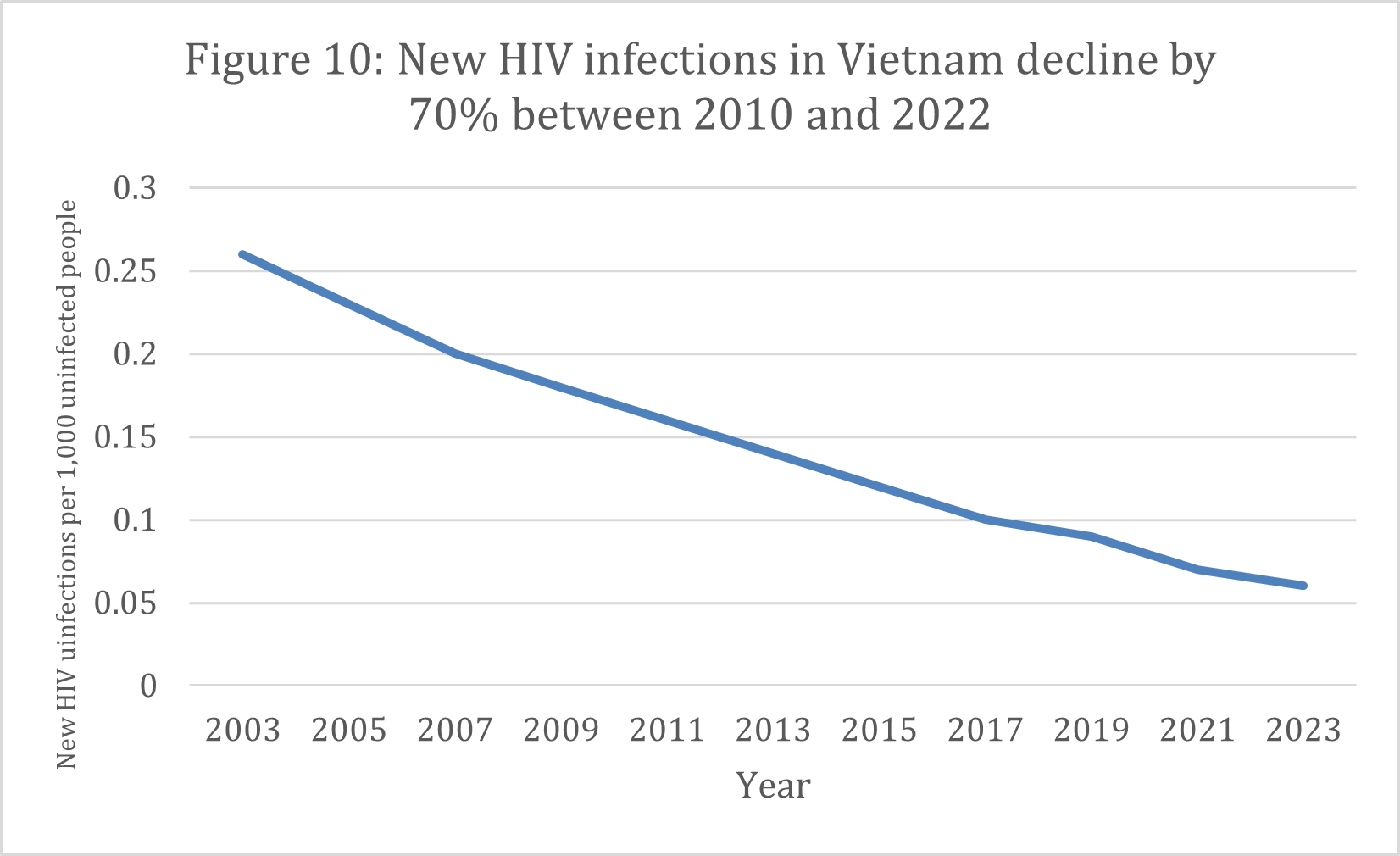
These policy changes paid off. Over the past decade, testing and knowledge of status among HIV-positive people in Vietnam grew to 94%, the treatment coverage among those with HIV increased to 78%, and viral load suppression rose to 73%. As more individuals learned their status and received treatment, the rate of new infections dropped as well, leading the annual number of new HIV infections to fall by 70% between 2010 and 2022 (Figure 10).
Not only are new infections declining, but AIDS-related deaths continue to fall as well. Vietnam represents one of the few HIV epidemics driven by key populations that has made this breadth of progress.
Source: UNAIDS
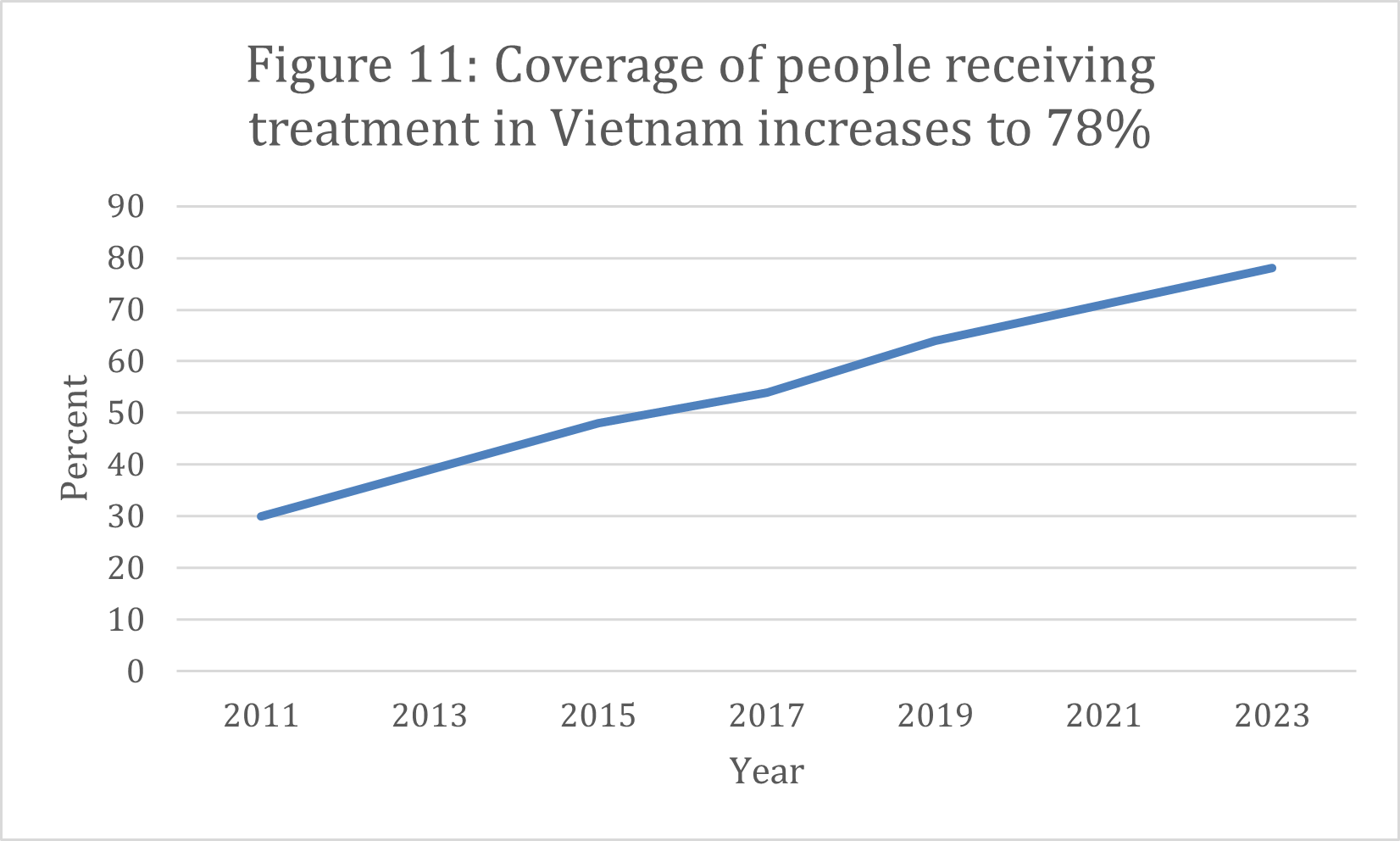
Recognizing the country’s capacity to fund more of the program, PEPFAR began discussions with the Vietnamese government about sustaining the HIV response. The Ministry of Health responded by providing HIV treatment as part of its national health insurance scheme. With significantly increased expenditures by the Vietnamese government, the number of people who receive ARTs has grown (Figure 11). PEPFAR has decreased its investment by 63%, from a high of $98 million in 2010 to $37 million in 2024.
Source: UNAIDS
Vietnam shows how PEPFAR’s strategy of partnership and sharing responsibility with national governments and communities can create a sustainable program. It also is a clear example of how policy and societal changes can ensure access to prevention and treatment by vulnerable populations. PEPFAR has a real opportunity to support the Vietnamese government in reaching the 95-95-95 goals by focusing on finding new HIV infections and helping the government rapidly put clients on treatment.
|
Vietnam |
||
| At least 95% of all people living with HIV should know their status (as of 2023) | At least 95% of all people with diagnosed HIV should receive ART and continue it (as of 2023) | At least 95% of all people on ART should have undetectable levels of the virus in their blood, known as viral load suppression (as of 2023) |
| 94% | 78% | 73% |

































