We Need to Explore Psychedelic-Assisted Therapy for Veterans
Veterans suffering from depression, post-traumatic stress and other invisible wounds are searching for effective treatments. The use of psychedelic-assisted therapy is no magic solution, but it deserves more exploration as one alternative for veterans in need.
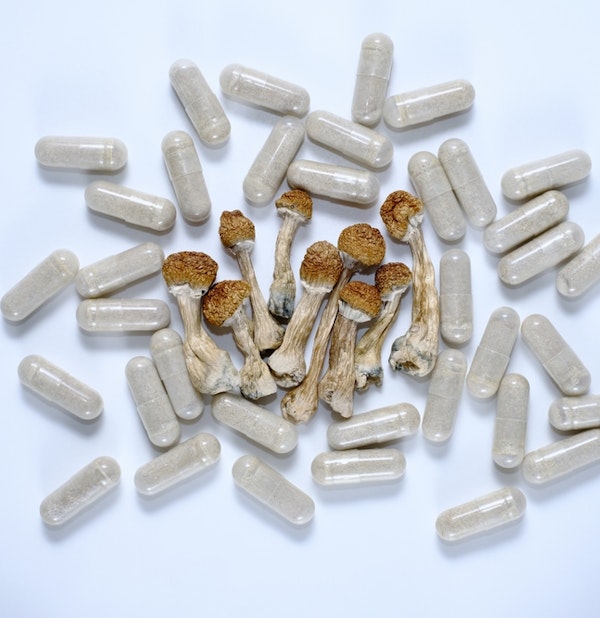 Micro-dosing concept with psilocybin mushrooms to help with mental health. (Shutterstock)
Micro-dosing concept with psilocybin mushrooms to help with mental health. (Shutterstock)
Margaret Harrell is Chief Program Officer at the Bob Woodruff Foundation. Colonel Matthew Amidon is the former Director of Veterans and Military Families at the George W. Bush Institute. Together, the pair participated in a discussion last year at an event the Bush Institute and Woodruff Foundation sponsored to advance health and well-being in the military and veteran community.
They engaged in a recent email exchange with Catalyst Editor William McKenzie about the entry of psychedelic drugs into treatment of U.S. veterans who might be suffering from their invisible wounds: depression, substance abuse, and post-traumatic stress. Neither considers such substances a “magic pill,” but they do contend that veterans are eagerly looking for solutions, including safe, effective use of psychedelic drugs.
Let’s start with the elephant-in-the-room. The term “psychedelic drugs” is likely associated in the minds of many Americans with the live-and-let-live culture of the 1960s. Now, some say the drugs perhaps can help veterans who suffer from post-traumatic stress, substance abuse, or depression. How have we reached this point?
Harrell: The live-and-let-live culture of the 1960s was actually a midpoint, not a beginning. These substances had shown promise in research previously, and then they “leaked” into the party environment, which prompted actions to banish them, make them illegal, etc.
Amidon: We have certainly reached a point where we need to address the reality that the term “psychedelic” elicits confusion and misunderstanding in creating policies and implementing treatment. By grouping the drugs into one bucket, the risk and potential for each is impacted. In the end, the core customer, the veteran in need and their family member, is actively looking for solutions and treatments.
Harrell: Absolutely right, Matt — and I also think that our collective memory only extends back to the period when this collective of “psychedelics” were crazy party drugs as per the question, and not research drugs.
So, what are these drugs? Are they the same kind that people used, as you said Meg, at the beginning?
Amidon: Some substances currently termed “psychedelic” have centuries-long histories of use while others are more recent. As important as the substance is the truth that within each, there are varied potencies and quality controls. This creates a problem for clinical delivery.
For example, MDMA, or “Ecstasy,” is commonly used in the veteran space and can exist from “street level” quality to clinical grade. Therefore, there can be barriers to their adoption and use within a clinical framework without the requisite research to determine the safest dosage and usage.
Harrell: “Psychedelics” include a broad range of chemical compounds, including both synthetic compounds (e.g., MDMA and LSD) and others that occur naturally or are produced from plants and fungi (e.g., psilocybin, mescaline, ayahuasca).
The substances differ from one another, so they vary in their efficacy and application. They show different degrees of promise treating PTSD, substance use, and depression, for example.
In the end, the core customer, the veteran in need and their family member, is actively looking for solutions and treatments. – Matthew Amidon
They have different contra-indications and implementation issues. And they are proceeding separately through research and approval stages. Also importantly, the research/pharmaceutical grade of these substances can differ significantly from the “street” grade.

What does the science say about the best way for veterans to use these substances effectively and appropriately?
Harrell: That varies by substance and also by application. Encouragingly, the research appears to show promise for PTSD, depression, and substance use disorder, all of which are especially prevalent in the veteran population. (PTSD at higher rates than civilians, depression at similar rates to civilians, substance use at slightly higher rates than civilians)
The consistency across most of these substances and applications is that it is psychedelic-assisted therapy that is effective. In the report that the Bob Woodruff Foundation and the Bush Institute published, we emphasize that psychedelics are NOT a magic pill.
Psychedelics-assisted therapy requires trained professionals to administer the substance, accompany the patient through the experience, and perhaps most importantly, to “unlock” the benefit of the substance. In some ways, the psychedelic substance is perceived to remove psychological barriers so that the psychotherapy can be more effective. In this way, the psychedelics may be enabling and increasing the efficacy of the therapy.
Amidon: The science indicates that, for many, psychedelics are one of many effective tools to address their invisible wounds. The individual in need has to stay focused on their health and well-being journey and acknowledge that, for most, psychedelics are not a singular “magic pill.”
Their use is best delivered alongside evidence-based care in a safe and trusting, culturally competent clinical setting. Correspondingly, clinicians and providers must acknowledge the importance of integrating the use of psychedelics into evidence-based care interventions alongside robust research into their safe use and efficacy.
You each have emphasized that these substances are not a magic pill. Are you concerned that they might be oversold as The Next Big Thing?
Amidon: Yes: There is an enduring narrative that veterans are “broken.” There remain systemic and individual barriers to those in need seeking care for mental and brain health.
Many simply are not taking the first step in seeking care and for those who do, many face confusion as to types of treatment available alongside varied quality of delivery of that treatment. This leaves them and their families frustrated and desperate and searching for anything that provides comfort.
Their searching, alongside a growing awareness of the use of psychedelics, may influence some to use them, and not engage in other evidence-based treatments that can enhance their health and well-being when appropriately integrated.
The consistency across most of these substances and applications is that it is psychedelic-assisted therapy that is effective. In the report that the Bob Woodruff Foundation and the Bush Institute published, we emphasize that psychedelics are NOT a magic pill.
– Margaret Harrell
Harrell: Absolutely! In fact, I think they’ve already been potentially oversold. What other product in American culture have people wanted so badly that, before they’ve been determined to be fully safe and efficacious, people have gotten on planes to other countries to consume?
The good news is preliminary results look like these substances provide important relief. But they haven’t been fully studied against other evidence-based therapies. So, we don’t have complete information about the benefits and the risks of these substances.
Even if they are risky, they may provide relief to individuals who have not responded to other treatments or therapies. But we don’t know enough to know whether their primary application should be to those resistant to other therapies, or whether we should administer psychedelic-assisted therapy more broadly. We don’t know enough to make risk assessments.
There are many efforts underway within the VA and the private sector to better understand the use of psychedelics and the role they can play. The risk is that this research and potential results are disparate and stove-piped.
— Matthew Amidon
Some proponents want them to be widely available, to save lives, even with some risk. Others want to understand the evidence and the risks, before proceeding. This is a big point of contention of those involved in the research, legislation, and policy.
Amidon: I like Meg’s answer. It highlights the fact that it’s not just psychedelics and those in need, it’s psychedelics and the system of care.
There are significant institutional barriers to promoting further research, and testing integration of psych-assisted therapies.
You all also have referenced policy implications. So, where are public policies headed in terms of using these substances to treat veterans?
Harrell: A lot of the activity right now is legislative, primarily at the state level. We’re seeing a hodgepodge of state laws about the use, research, and sale of these substances. And even within states, we’re seeing some localities setting different restrictions. RAND recently published a good summary of this activity.
Policy-wise, the most important player in this discussion is the VA. The department has consistently led research on health issues that impact the entire country, and it has invested in research pertaining to psychedelics.
To date, they’ve taken a steady but relatively cautious approach to studying psychedelic-assisted therapy, adherent to federal rules. Most recently, they published an evidence brief underscoring the need for additional research before they can proceed with treatment guidance or policy decisions.
Amidon: Policy implications start with research and understanding to drive informed action. There are many efforts underway within the VA and the private sector to better understand the use of psychedelics and the role they can play. The risk is that this research and potential results are disparate and stove-piped.
The key question is how will the research be aggregated and synthesized at the system level across the array of treatment options so that care providers in our communities can best understand need, risk, and opportunity. There is much promise here and it’s time to stop using an unfortunate label on an array of treatments that have shown true promise.
Harrell: I really like Matt’s answer about the stove-pipes.
Two questions in one here: Is the veteran community ready for this shift in the use of such drugs? And is the public?
Amidon: The veteran community is already there and willing to take bold steps to address those in need and their families. The American public, with views now shifting on topics like decriminalization and legalization of substances like marijuana, is ready and open for a candid discussion on the research into, and use of, tools and therapies that help those in need maintain their quality of life.
The general public has not been privy to that same groundswell of information, and they need to be more informed before they’ll be ready.
— Margaret Harrell
Harrell: Veterans are ready, eager, and impatient. We’ve seen that many are willing to circumvent the process to ensure that these drugs are safe and efficacious, because word has spread about the effectiveness of these drugs and the relief they provide.
The general public has not been privy to that same groundswell of information, and they need to be more informed before they’ll be ready. Many in the public still react with an emotional negative response to “psychedelics” because they associate these substances with the lore of the party drug. Those who are informed about the therapeutic opportunities of these substances become ready. But that’s not yet the general public.
The Catalyst believes that ideas matter. We aim to stimulate debate on the most important issues of the day, featuring a range of arguments that are constructive, high-minded, and share our core values of freedom, opportunity, accountability, and compassion. To that end, we seek out ideas that may challenge us, and the authors’ views presented here are their own; The Catalyst does not endorse any particular policy, politician, or party.
-
Previous Article We Owe Native American Veterans a Better Health Care System Essay by Matthew Brogdon, Founder and Executive Director of Hesperus
-
Next Article It Takes a System Interview with Alex Gorsky, the April and Jay Graham Fellow at the Bush Institute and Former Chairman and CEO of Johnson & Johnson



